Pancreatic Treatment In Hyderabad

What Is Pancreas?
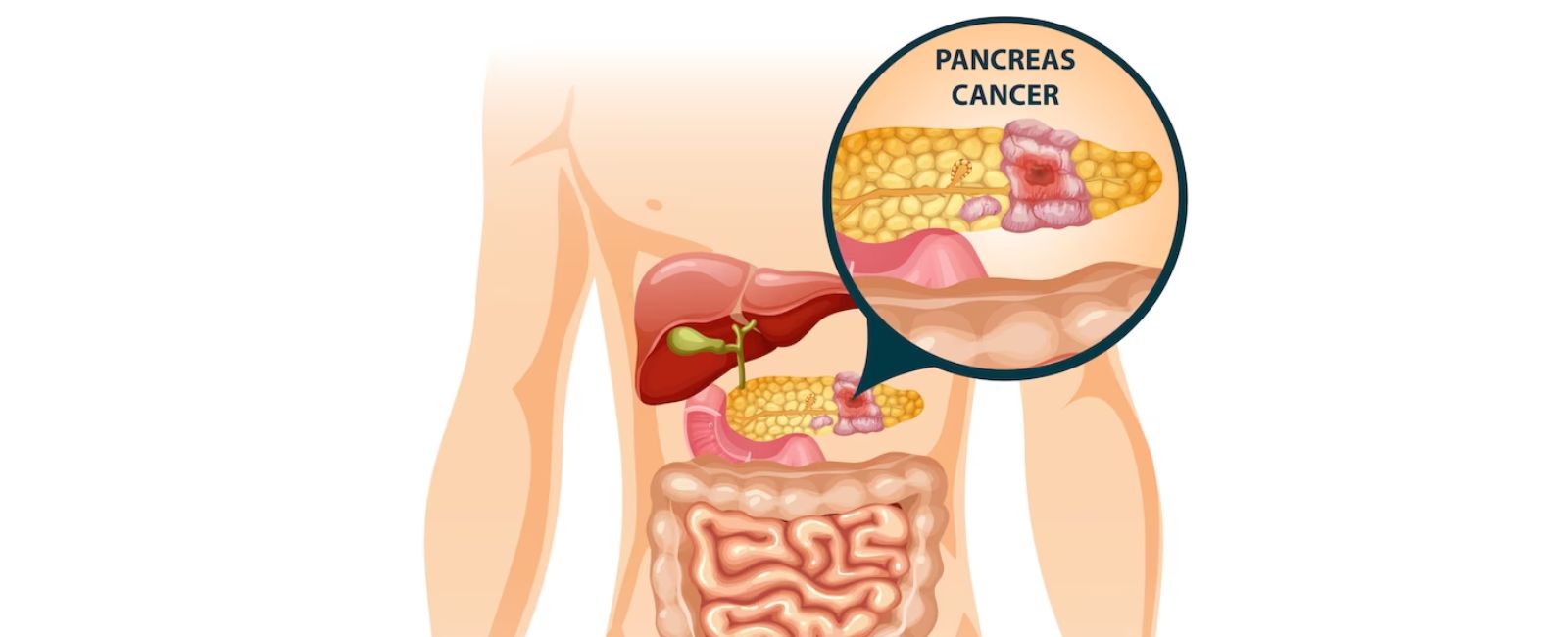
The pancreas is a vital organ located in the abdomen, specifically behind the stomach and in front of the spine. It plays a crucial role in digestion and the regulation of blood sugar levels.
The pancreas has two primary functions:
Exocrine Function: The majority of the pancreas consists of exocrine cells that produce digestive enzymes. These enzymes are released into the small intestine to help break down proteins, fats, and carbohydrates from the food we eat. The enzymes include amylase, lipase, and proteases, which aid in the digestion and absorption of nutrients.
Endocrine Function: Scattered throughout the pancreas are small clusters of cells called the Islets of Langerhans. These cells have an endocrine function and are responsible for producing and releasing important hormones into the bloodstream. The two main hormones produced by the pancreatic islet cells are insulin and glucagon. Insulin helps regulate the levels of glucose (sugar) in the blood by facilitating its absorption into cells for energy or storage. Glucagon, on the other hand, raises blood sugar levels by promoting the breakdown of stored glycogen in the liver.
Understanding Pancreatic Conditions:
The pancreas plays a crucial role in digestion and hormone production. Pancreatic conditions can encompass a range of disorders, including:
- Pancreatitis: Inflammation of the pancreas, which can be acute or chronic, often caused by alcohol abuse, gallstones, or certain medications.
- Pancreatic Cancer: The uncontrolled growth of malignant cells in the pancreas, which can be challenging to detect at early stages and requires specialized treatment.
- Pancreatic Cysts: Fluid-filled sacs that form in or on the pancreas, which may or may not be cancerous and might require intervention based on their size and characteristics.
- Pancreatic Neuroendocrine Tumors (PNETs): Rare tumors that develop from hormone-producing cells in the pancreas, requiring a multidisciplinary approach for diagnosis and treatment.
- Pancreatic Pseudocysts: Fluid collections that form after acute pancreatitis or pancreatic trauma, which may require drainage or intervention if they cause symptoms.
What are the types of pancreatitis?
There are two types of pancreatitis:
Acute Pancreatitis: This is a sudden and severe inflammation of the pancreas that occurs quickly and lasts for a short period of time. Symptoms include severe abdominal pain, vomiting, and high fever.
Chronic Pancreatitis: This is a long-term and recurring inflammation of the pancreas that occurs over time and may cause permanent damage to the gland. Symptoms include abdominal pain, weight loss, and digestive problems. Chronic pancreatitis may also lead to complications such as diabetes and malnutrition.
What causes pancreatitis?
Here are some of the common causes of pancreatitis:
- Alcohol abuse: Excessive alcohol consumption is the most common cause of acute pancreatitis.
- Gallstones: When gallstones block the duct that carries digestive enzymes from the pancreas to the small intestine, it can cause inflammation in the pancreas.
- High levels of fat in the blood: High levels of fats in the blood, such as triglycerides, can lead to pancreatitis.
- Certain medications: Some medications, including steroids, diuretics, and high doses of thiazolidinediones (used to treat diabetes), can cause pancreatitis.
- Abdominal surgery: After abdominal surgery, particularly surgery involving the gallbladder, bile duct, or pancreas, pancreatitis can develop.
- High calcium levels: High levels of calcium in the blood can cause pancreatitis.
- Viral infections: Certain viral infections, such as mumps, can lead to pancreatitis.
- Pancreatic cancer: Pancreatic cancer can cause inflammation in the pancreas, leading to pancreatitis.
- Autoimmune disorders: Certain autoimmune disorders, such as lupus or rheumatoid arthritis, can cause pancreatitis.
- Trauma: Trauma to the pancreas, such as from a car accident, can cause pancreatitis.
Types of Pancreatic Surgery:
Pancreatic surgery is a complex procedure that is performed to treat various conditions related to the pancreas, such as pancreatic cancer, pancreatitis, and cysts. There are several types of pancreatic surgeries, each with its own set of benefits and risks.
Here are the different types of pancreatic surgeries:
1). Whipple Procedure (Pancreaticoduodenectomy): This is the most common type of pancreatic surgery performed to treat pancreatic cancer. The procedure involves the removal of the head of the pancreas, the duodenum, the gallbladder, and the bile duct. This procedure is used to treat early-stage pancreatic cancer and is considered a cure for some patients.
2). Distal Pancreatectomy: This procedure involves the removal of the body and tail of the pancreas. It is typically performed to treat cystic tumors, benign tumors, and chronic pancreatitis.
3). Total Pancreatectomy: This procedure involves the removal of the entire pancreas, including the head, body, and tail. This procedure is usually reserved for patients with severe chronic pancreatitis or for patients with a rare type of pancreatic cancer.
4). Pancreatic Resection: This procedure involves the removal of a portion of the pancreas. It is typically performed to treat benign or malignant tumors that are located in the head, body, or tail of the pancreas.
5). Laparoscopic Pancreatic Surgery: This is a minimally invasive procedure that is performed using small incisions and specialized instruments. The procedure is typically performed to treat benign or malignant tumors, and it is considered less invasive than traditional open surgery.
Each type of pancreatic surgery has its own set of benefits and risks, and the appropriate procedure will depend on the patient’s specific needs and medical condition. Before undergoing pancreatic surgery, it is important to have a thorough consultation with a qualified specialist who can help you understand the procedure, its benefits, and the risks involved.
Frequently Asked Questions(FAQ)
What are the symptoms of pancreatic diseases?
What are the functions of the pancreas?
What is the significance of insulin and glucagon?
Where can I seek specialized care for pancreatic conditions?
Where is the pancreas located?
How are pancreatic diseases diagnosed?
What are the treatment options for pancreatic conditions?
What are some common pancreatic conditions?
Success Stories
A true Master in his job!!! His expertise, care, calm approach towards patients & family - I just liked everything about Dr. Jagan Sir.
Meet Our Specialist
Dr. B Jagan Mohan Reddy is an experienced Gastroenterologist Surgeon in Hyderabad with an overall experience of 14 years.
Dr B Jagan Mohan Reddy
drjagangastrocare.com
MBBS,MS, M.CH Consultant Surgical Gastroenterologist, Laparoscopic, Bariatric, Advanced Robotic, Colorectal, Hepato Biliary & Pancreatic Surgeon

